Among diabetes complications, diabetic foot is one of the most easily overlooked yet most dangerous conditions. Once ulcers, infections, or tissue necrosis occur, the consequences range from impaired walking to, in severe cases, amputation. In fact, 80% of diabetic foot lesions show signs early on.
How can these “hidden dangers” be detected in advance?
One answer lies in plantar pressure plate monitoring.
Today, let’s discuss how plantar pressure plates can accurately identify high-risk areas for diabetic foot, enabling early warning and early intervention.
1. The root causes of diabetic foot: neuropathy + abnormal pressure
Diabetic patients often suffer from peripheral neuropathy, resulting in reduced or lost sensation in the soles. This leads to decreased sensitivity to pressure and pain signals. A small corn or blister, if unnoticed and subjected to continuous pressure, can develop into an ulcer.
At the same time, muscle atrophy in the foot and gait changes cause abnormal local pressure, forming “high-pressure points” that are common sites for lesions due to prolonged concentrated stress.
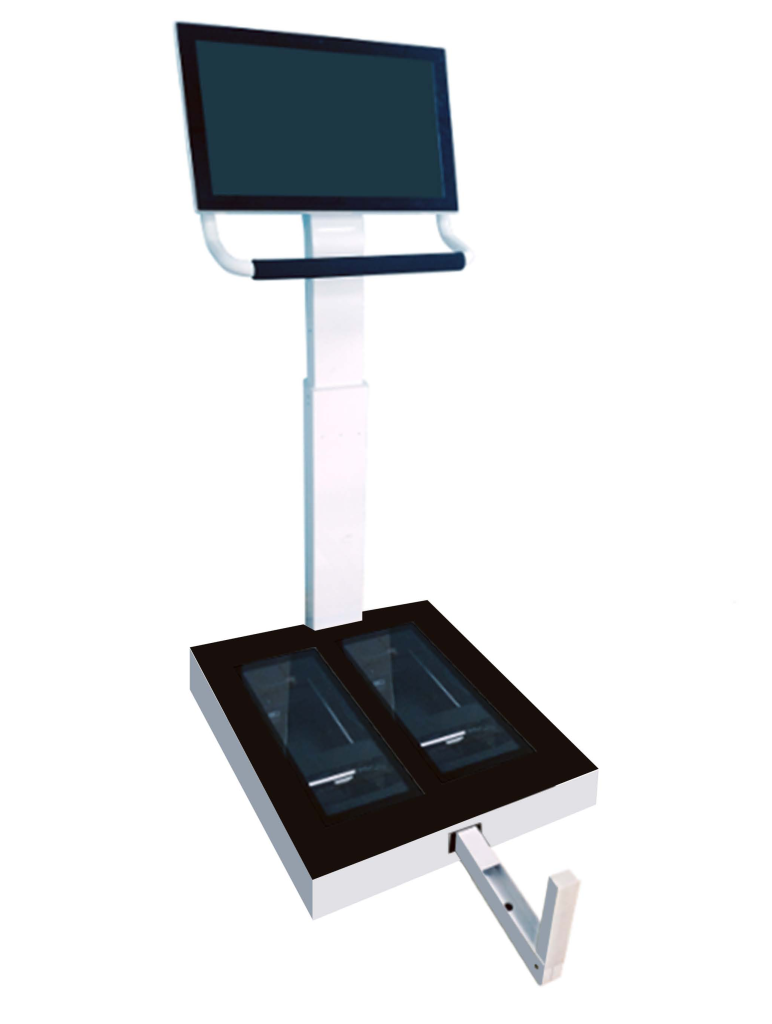
2. Plantar pressure plates: a mat that “sees through” risks underfoot
A plantar pressure plate is a highly sensitive device embedded with thousands of micro pressure sensors. Patients simply stand or walk on it, and the system records real-time pressure changes across every part of the sole.
Core functions include:
High-pressure point identification: Detects localized pressure concentrations on the forefoot, heel, etc.
Contact time analysis: Evaluates whether certain areas endure prolonged pressure.
Center of pressure (COP) trajectory shift: Assesses whether gait abnormalities cause excessive compensation in specific regions.
Left-right foot symmetry comparison: Identifies hidden compensatory gait patterns or unilateral disease tendencies.
3. Guide to interpreting high-risk area characteristics
Forefoot pressure concentration: Common in cases of fallen arches or improper walking; a hotspot for ulcers.
Heel single-point high pressure: May be related to insufficient shoe sole support or abnormal heel posture.
Toe pressure loss: Indicates severe peripheral nerve sensory impairment, increasing risk of unnoticed wounds.
Abnormal COP trajectory deviation: Suggests chronic pressure points from long-term unilateral compensation.
Using these data, clinicians can develop targeted orthotic insole designs, gait corrections, or offloading strategies to reduce ulcer incidence from the root.
4. Technical application advice: regular monitoring + personalized intervention
For diabetic patients—especially those with foot numbness, deformities, or prior injuries—it is recommended to perform plantar pressure monitoring every 3 to 6 months. Combined with orthotic insoles, offloading footwear, and gait training, these interventions form a comprehensive approach.
